The most common diseases in men over the age of 40 are prostatitis and hemorrhoids. Moreover, in some cases, both diseases can develop in parallel, which greatly impairs the quality of human life. Here you need to find out what these two diseases are and what the symptoms are in order to recognize the problem on your own and consult a specialist in time.
What is hemorrhoids: features and symptoms
Hemorrhoids are enlarged veins in the rectum. These veins are called hemorrhoids and when they dilate they form lumps.
The main cause of the disease is a violation of the outflow of blood from the lower rectum. There are various reasons for this:
- sedentary lifestyle;
- overweight;
- frequent constipation;
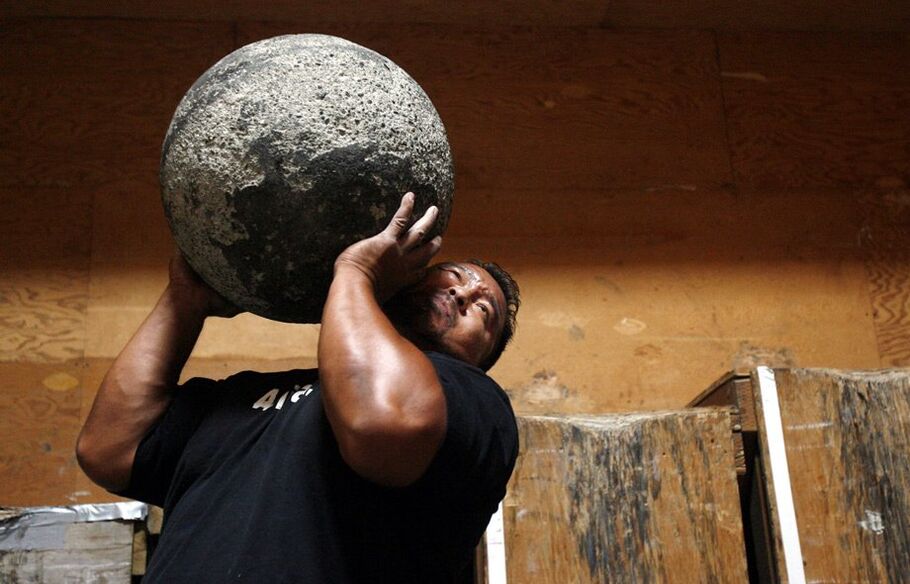
- overload;
- inflammation of the rectum.
That is, the blood rushes to the area of the hemorrhoids, but its outflow is damaged, so it overflows the veins, which dilate. Due to the dilation of the veins, there is a change in the tissue of the corpora cavernosa below the rectal mucosa. These sections swell and grow, and so-called hemorrhoids develop.
Nodes can be internal or external. The external nodes are the result of weakening of the sphincter muscles, causing the internal nodes to move and fall out of the anus. The number of internal or external formations in the rectum can vary from one to several nodes. Moreover, the more nodes, the more severe the symptoms of the disease.
Hemorrhoids are most commonly associated with chronic, intermittent exacerbations.
The disease progresses slowly, with symptoms remaining invisible for a long time, which explains the main problem with hemorrhoids - late diagnosis. In the initial stage, the symptoms are mild:
- mild edema of the tissues of the lower rectum;
- intermittent itching in the anus;
- burning and aching pain after stool.
Symptoms are aggravated by constipation - severe pain and stinging occurs during defecation. At the same time, secretions may be released from the rectum, which further irritates the mucous membranes, enhancing the burning sensation.
Expressed hemorrhoids are manifested by inflammation of the nodes. This is accompanied by unbearable pain. Nodes are damaged during defecation, so there is blood in the stool.
Over time, the cavernous bodies of the rectum can become severely deformed, resulting in knots falling out and being literally secured with your fingers in the anus.
Basic concepts of prostatitis

Prostatitis is an inflammation of the prostate. This disease can occur in both acute and chronic infectious and non-infectious forms.
If prostatitis and hemorrhoids are considered at the same time, special attention should be paid to the non-infectious chronic inflammatory process in the prostate gland. This disease is often referred to as stagnant prostatitis.
The crux of the problem lies in the violation of the trophism of the prostate gland. By trophism is meant blood microcirculation and lymph outflow. The deterioration of these processes leads to the following changes:
- the secret of the prostate gland stagnates;
- the organ swells;
- the secretion in the prostate thickens;
- an inflammatory process develops.
The violation of trophism results in swelling and enlargement of the prostate, which compresses the surrounding tissues and organs (the neck of the bladder, the lower part of the urethra), resulting in vivid symptoms of prostatitis.
The main causes of congestive prostatitis are:
- sedentary lifestyle;
- lack of regular sex;
- overweight;
- bad habits;
- unbalanced diet.
Usually, men over the age of 40 face this disease.
Doctors often refer to congestive prostatitis as an "office worker disease, " thus emphasizing the link between a violation of prostate trophism and a sedentary lifestyle.
The symptoms of the disease are as follows:
- frequent urge to use the toilet;
- pain in the perineum, rectum, bladder;
- impaired urine flow during urination;
- a feeling of a constantly full bladder;
- ejaculatory disorders;
- deterioration of potency.
Ejaculatory disorders are manifested by either rapid ejaculation with short-term stimulation of the penis or an inability to reach orgasm during intercourse. The first involves an increase in the tone of the prostate, the second - a violation of the contractility of the organ.
What connects prostatitis to hemorrhoids?

The link between prostatitis and hemorrhoids is obvious - common causes of development. And in one case or another, the disease is caused by damage to the bloodstream and lymphatic circulation. In this case, the inflammation of the prostate causes a thickening of the juice in the prostate due to a violation of trophism, and hemorrhoids develop due to a violation of the venous outflow of blood from the rectum.
The following reasons lead to such violations:
- sedentary lifestyle (sedentary work);
- lack of regular sex;
- obesity;
- bad habits.
Most modern people work in an office, meaning they spend most of their time sitting. In the conditions of modern life, few people find enough time for active recreation and sports, and spend most of the day in a sitting position. The result is poor circulation in the pelvis and lower extremities. However, if a man has problems with the veins in his leg, the problems with the pelvic organs are only a matter of time. In general, varicose veins are also found in an age group at risk of developing prostatitis.
Lack of regular sex seems to only affect the prostate, but what has this got to do with hemorrhoids? This is exactly the case when both diseases are associated and the development of congestive prostatitis is associated with dilation of the hemorrhoid veins. Bad sex life negatively affects prostate function. As a result, congestion develops and symptoms of prostatitis appear. An enlarged prostate presses on surrounding tissues, including blood vessels, disrupting normal blood flow in this area. As a result, the rate of blood flow to the veins of the rectum changes, venous stagnation gradually develops, the veins dilate, and hemorrhoids form. Of course, this process takes years, but if we do nothing, prostatitis will eventually lead to hemorrhoids.
The same thing happens with obesity. The trophism of the pelvic organs is damaged and inflammation of the prostate or hemorrhoids develops. If the man has not responded in any way to the presence of one of these diseases, the development of the second should be expected over time.
The negative effects of bad habits need to be considered separately. The most common addictions are smoking and alcohol consumption. Nicotine has a negative effect on blood vessels, increasing their tone. As a result, they narrow, which negatively affects the rate of blood flow. Another factor is the disruption of oxygen delivery to tissues during prolonged smoking. The result will again be poor circulation in the pelvic organs and lower extremities, leading to congestion, inflammation of the prostate or hemorrhoids.
Alcohol consumption negatively affects the functioning of the nervous system and cardiovascular system. An increase in blood pressure is often observed, which is the cause of impaired blood flow. Thus, smoking and systematic alcohol consumption are a direct pathway for the development of prostatitis and hemorrhoids.
Usually, one of these diseases is caused by several factors at the same time. Over time, congestion spreads to all the organs in the pelvis, causing a second disease to develop.
Once you’ve figured out if hemorrhoids are linked to prostatitis, you need to know that both diseases can develop in parallel. The presence of two of these diagnoses complicates treatment, so you should see a doctor immediately.
Treatment of hemorrhoids and prostatitis
If both diseases have worsened, they should be treated at the same time. In general, the treatment of these two diseases overlaps somewhat, so taking medication can stop exacerbation.
Tablets and suppositories are used to treat inflammation of the prostate. Rectal suppositories are also used to treat hemorrhoids, and microclysters are added to the therapy.
Cones
Mild anti-inflammatory agents are preferred. At the same time, they stop the inflammation of the prostate and reduce the manifestations of hemorrhoids.
In addition, methyluracil suppositories may be recommended to improve local metabolic processes and enhance immunity. Suppositories containing ichthyol are often prescribed as anti-inflammatory agents.
Microclysters to relieve inflammation
Microclysters are used both to stop the inflammatory reaction and as an intestinal preparation before administering suppositories. At home, the enema is made with a decoction of anti-inflammatory herbs - chamomile, St. John's wort, marigold.
Physiotherapy and gymnastics
Physiotherapy is prescribed only after the relief of acute symptoms. It aims to improve blood circulation in the pelvic organs and can reduce the frequency of exacerbations. Electrostimulation, magnetotherapy, and laser therapy are used to treat prostatitis.
Because access to the prostate occurs through the rectum, such procedures have a positive effect on the health of the anus.
Practical therapy is prescribed to any man who faces stagnant processes in the pelvic organs. Exercise stimulates local circulation and lymphatic drainage. They can be performed at the clinic or at home. In addition, men benefit from sports, swimming, yoga, and moderate pace running.
Prostate massage for hemorrhoids
Prostate massage is the best treatment for congestive prostatitis, which is strictly contraindicated in case of hemorrhoid inflammation in the background of worsening hemorrhoids. Procedures should be postponed until the inflammation of the nodes has ceased. Otherwise, hemorrhoids can be damaged during the massage, leading to heavy bleeding and even spreading the inflammatory process or even infecting the site.
Preventive measures

The prevention of hemorrhoids and prostatitis is aimed at increasing the duration of remission and reducing the frequency of exacerbations. Preventive measures:
- balanced diet;
- constipation prevention;
- strengthening the immune system;
- to exercise;
- regular sex life;
- rejection of bad habits.
It is important to structure your diet to avoid constipation. Constipation is one of the main factors in the worsening of hemorrhoids and prostatitis as it impairs blood circulation. During bowel movements, hard stools cause injury to the rectum and hemorrhoids, causing aggravation and irritation to the prostate hidden by a thin hedge. Your doctor may also prescribe special medicines to prevent constipation, such as glycerin suppositories.
























