Description of the causes, symptoms, diagnosis, and treatment of acute or chronic bacterial prostatitis. Recommendations from urologists who help identify the disease quickly and contact the clinic in a timely manner to diagnose and prescribe complex therapy.
Prostatitis is one of the most common urological diseases in men. Inflammation of the prostate causes discomfort in life and can lead to sexual weakness.
According to various estimates, after a quarter to a third of the male population, the prostate will have a problem after 40 years, with statistics better among young people but still unhappy.
Today we talk about bacterial prostatitis (BP), examine its causes, symptoms, and the characteristics of diagnosis and treatment.
Causes of Occurrence
The complexity of PD is that it often progresses in a subtle form and is not detectable for a long time, delaying the start of treatment.
The main cause of bacterial inflammation of the prostate is infection of the gland, but not only does it lead to the disease.
Among the causes of bacterial prostatitis, note the following:
- Sedentary lifestyle.
- Violation of the rhythm of sex.
- Overweight.
- Chronic constipation.
- Alcohol consumption.
To understand how these causes affect the development and development of pathology, consider their specificities.
Microbes and infections enter the prostate regularly, but this does not always lead to bacterial infection because the immune system is working.
In addition, good blood flow quickly eliminates infections and stimulates local immunity in the gland area, which prevents infection.
Interesting!With a sedentary lifestyle and irregular sex, the prostate becomes congested, which is another factor in the development of the disease.
If you have a sedentary job, it is a good idea to go to the gym or exercise your hips at home after 40 and earlier.
Obesity and chronic constipation also interfere with blood flow in the gland area. Keep track of your weight and include high-fiber foods in your diet to prevent constipation.
As for alcohol, it weakens the immune system (with regular abuses), which removes the body’s protective barrier and makes it easier for microbes to “establish” the prostate.
Keep in mind that bacteriological prostatitis does not happen out of nowhere, it is most common in people who do not monitor their health.
Symptoms of the disease
Like any other disease, PD has its own symptoms, the severity of which varies depending on the stage of the disease and the characteristics of the patient's body.
Most often, a person with inflammation of the prostate is concerned:
- Frequent urination.
- Painful feelings when going to the toilet.
- Difficulty in the lumbar region.
- Decreased libido, even to erection problems.
The most striking symptoms occur when acute PD develops, if treatment is not started, the disease becomes chronic and the severity of the symptoms subsides.
There is no need to rejoice here, as chronic inflammations are more difficult to treat and therapy takes more time.
Important!If you have the first symptoms of prostatitis, this is a reason to see a urologist and diagnose it, because starting treatment quickly increases your chances of success.
Bacteria that cause inflammation of the prostate are microplasma, chlamydia, and other microbes that can enter the prostate through the bloodstream through urine or the primary infected organ.
Acute prostatitis
In acute form, the patient may experience a fever of up to 40 degrees and a fever. Lumbar pain can be sharp, purulent discharge from the urethra, and efforts to use the toilet are very common.

Acute bacterial prostatitis in men cannot go unnoticed, this is an advantage as the patient sees a urologist immediately.
In acute form, there is a strong burning sensation when visiting the toilet and general irritability and fatigue.
If treatment is not started on time, PD can lead to complications:
- Abscess in the body of the prostate.
- Vesiculitis.
- Colliculitis.
- Cicatricial changes in the prostate.
Abscess, on the other hand, can lead to rupture of the prostate and severe poisoning of the body, in the case of vesiculitis, pus appears in the sperm and human reproductive function can cease.
is no less dangerous for colliculitis, in which severe pain syndrome develops during sex, which can lead to psychological trauma and impotence.
Cicatricial changes lead to infertility as they reduce sperm motility and sperm quality. In addition, narrowing of the urethra with scars makes it difficult to urinate and leads to blockage of the bladder, which can be a reason for surgeon intervention.
Chronic form
Chronic bacterial prostatitis is primary or secondary. In the first case it develops immediately without an acute phase, in the second it occurs as an advanced form of acute inflammation of the prostate.
The symptoms of the chronic phase are more obscure, but they also cause discomfort to the patient:
- Difficulty urinating.
- The desire to use the toilet is growing.
- Erectile function is impaired.
- Burns and heaviness are felt in the perineal region.
These are the main signs of chronic PD, if treatment is not started on time (complex therapy), complications are possible in the following forms:
- Cystitis.
- Sepsis.
- Pyelonephritis.
- Decreased immunity.
The danger of the disease lies precisely in the less pronounced symptoms, which men sometimes simply ignore.
If it is impossible not to notice the acute phase, the chronic inflammatory process is often overlooked and treatment is then long and not always effective.
Diagnosing inflammation
When the first signs of prostatitis appear, you should see a doctor who will prescribe a series of diagnostic measures. They make it possible to determine the presence and type of inflammation that aids in the effective treatment of the disease.
The complete diagnostics include:
- Digital examination of the prostate gland.
- Analysis of prostate secretion.
- Lubrication for STDs.
- Ultrasound of the gland.
Your doctor may also order a sperm analysis and biopsy to rule out or confirm the presence of cancer in the prostate.
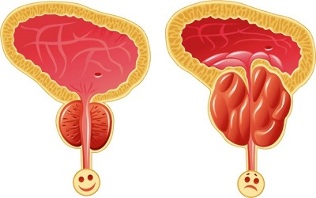
Digital examination of the gland is an inconvenient but important phase of diagnosis because the patient is simple, uneven in density, and enlarged.
Secretion analysis determines the infectious or non-infectious form of the disease, and ultrasound allows the doctor to see the contours of the gland - if they are blurred, it obviously confirms prostatitis.
After diagnosis, the urologist will decide on the patient's treatment, taking into account the following:
- Type of prostatitis.
- The form of the disease.
- Age of the patient.
- Individual characteristics of the patient.
- Presence of comorbidities.
Accurate diagnosis allows the selection of the optimal treatment regimen and the therapy shows the maximum effect. The more stages required for diagnosis, the more accurate the diagnosis will be and the easier it will be to prescribe a complex therapy.
Prostate Inflammation Treatment
Therapies for acute and chronic bacterial prostatitis are different because they require different doses of medication and the duration of treatment is different.
Interesting!In the initial stage, it is important to eliminate the unpleasant symptoms for the patient in order to improve the quality of life, since it is the doctor's job to get rid of the disease completely, regardless of its form.
Acute prostatitis therapy

Ethiotropic therapy must be prescribed for the treatment of acute prostatitis, antibiotics and antimicrobials should not be used in bacterial diseases.
In addition, the following are assigned:
- Analgesics.
- Immunostimulants.
- Vitamins with trace elements.
- Massage.
Drugs for PD are selected individually depending on the primary infection and the course of the disease.
Important!Antibiotics and antibacterial agents fight bacteria, while vitamins and immunostimulants help boost immunity.
Acute pre-acute massage promotes the clearance of prostate secretion and normalizes gland blood flow.
Massage should not be prescribed in the event of an acute illness and physiotherapy procedures such as laser and electrophoresis are not recommended at this stage.
Mandatory phase of treatment but not recommended in the acute phase of PD.
Chronic prostatitis therapy
Treatment of chronic bacterial prostatitis requires longer therapy and extended procedures. It is often necessary to increase the dose of drugs.
Added to the above stages of treatment:
- Taking herbal medicines.
- The full range of physiotherapy.
- Perform special exercises.
- Consultation with a psychologist.
As potency decreases, an increased dose of vitamins and stimulants may be prescribed as treatment requires regular sexual activity.
As far as practices are concerned, they are selected depending on age, disease course, and individual characteristics of the body. Your doctor will also consider the presence of side effects.
You learned from the article how to diagnose bacterial prostatitis, and then you just need to pay close attention to your health and see a doctor when the first signs of the disease appear.
The sooner therapy begins, the shorter the treatment process and the sooner the man will return to full life.
























